
Back to Articles
Blood Work Results: What’s Normal vs Worth Following Up
Blood work results explained: what “normal” means, which abnormal patterns matter, and how to decide when to retest or follow up with a clinician.
Blood Test Interpretation
January 31, 2026
1 min read
Vitals Vault Team
Core Essential Wellness Panel
100+ Biomarkers & a thumbprint of your biological age
Includes the depth of physician-backed labs plus AI-reviewed storytelling so you can act on your physiology with confidence.
- 100+ doctor-curated functional medicine tests
- Personalised Action Plan + AI-reviewed clinical summary
- Upload, track, and securely share past reports
- PhenoAge score to measure your biological age
Understanding your blood work results can be confusing, especially when lab reports show abnormal flags but you feel fine, or vice versa. This post explains what "normal" means in lab results and helps you differentiate between common fluctuations and results that deserve medical follow-up. It covers key blood markers, patterns to watch, and practical steps to prioritize which abnormalities in your blood work results should be addressed.
Your blood work results can feel oddly contradictory: the lab report shows bold flags and “H” or “L” markers, yet you feel fine. Or everything looks “normal,” but you do not feel like yourself.
The goal is not to panic over a single number. It is to separate normal variation from signals that deserve follow-up, then decide what the next best step is (retest, add a companion marker, or talk with a clinician soon).
First, what “normal” actually means on a lab report
Most reports show a reference range, sometimes called the “normal range.” That range is usually built from results in a large group of generally healthy people, often capturing the middle 95%.
That has three important implications:
- “Normal” does not always mean “optimal for you.” It means your value is common in the reference population.
- A value slightly outside the range can happen in healthy people. By definition, some healthy results fall outside a 95% range.
- Ranges vary by lab, method, age, and sex. Always interpret the number using the reference range printed on your report.
If you want a solid primer on how labs define and display results, MedlinePlus offers a clear overview of how to understand medical test results.
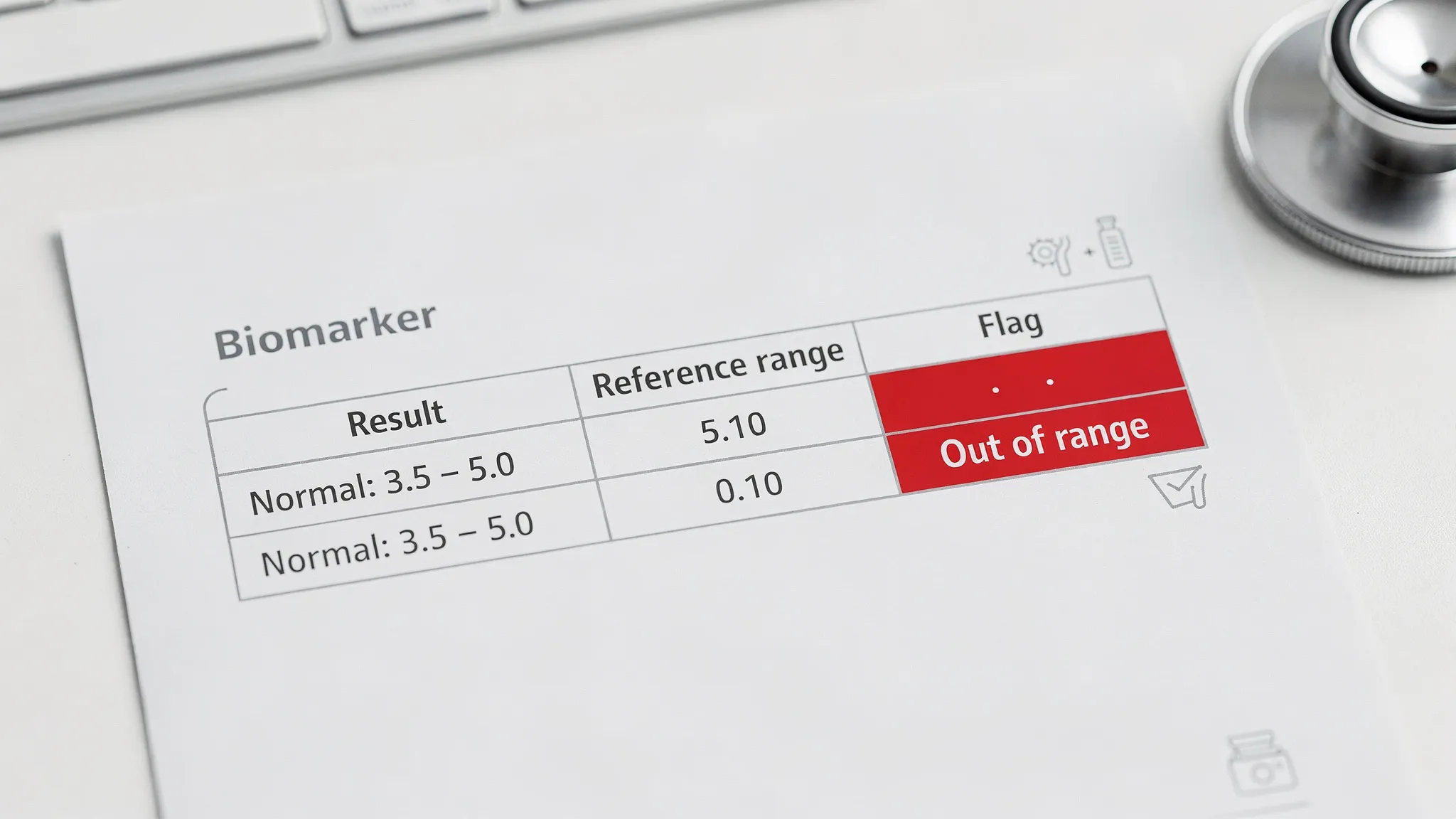
Why blood work gets “flagged” when you might be fine
A flagged result can be real, but it can also be temporary or explainable. Common reasons include:
- Timing and prep: fasting status, time of day, recent alcohol, a hard workout, poor sleep.
- Hydration: dehydration can concentrate some values.
- Acute illness: even a mild virus can shift inflammatory and immune markers.
- Medications and supplements: from NSAIDs to creatine to biotin, many can affect labs.
- Normal biological variability: your body fluctuates.
A useful rule: one abnormal result is a clue, not a diagnosis. Patterns and trends carry more meaning than a single data point.
A practical triage: what’s normal vs worth following up
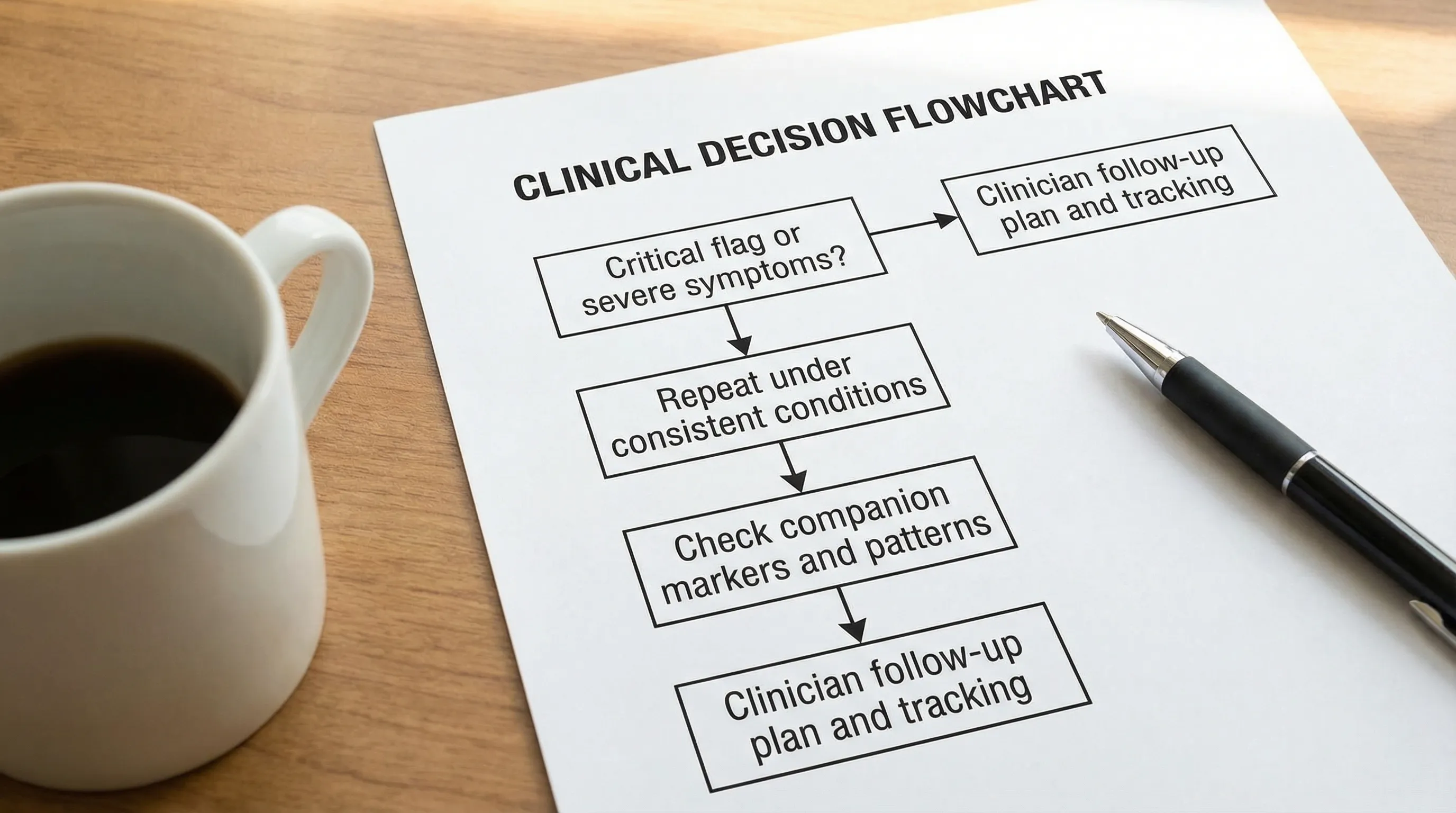
If your report shows “critical” values, follow the lab’s instructions immediately. Many labs attempt direct outreach for critical results because they can require urgent care.
For everything else, this framework helps you prioritize.
Swipe
The “pattern” approach: how clinicians make labs make sense
Instead of asking “Is this number normal?” ask:
- Is it new for me? Compare to prior labs.
- Is it persistent? A repeat test often distinguishes a fluke from a trend.
- Does it match other markers? One marker rarely tells the full story.
- Does it match symptoms or risk factors? Numbers matter more in context.
Below are the most common areas where blood work results are either “normal enough” or worth following up, with a focus on patterns that change decisions.
1) Complete Blood Count (CBC): when “a little off” matters
CBC results generate a lot of flags. Many are benign, but certain combinations deserve follow-up.
WBC and differential: infection, inflammation, or recovery
A slightly high white blood cell count after poor sleep, stress, or a recent infection is common. What is more informative is whether the elevation is persistent or paired with other changes (like shifts in neutrophils or lymphocytes).
If you want to go deeper on what WBC patterns can mean, Vitals Vault has a dedicated guide to WBC count.
Worth following up:
- WBC abnormalities that persist on repeat testing
- Abnormal differential patterns that do not match how you feel
- Very low WBC, or recurrent infections along with low counts
Hemoglobin and hematocrit: anemia vs “thick blood” patterns
Low hemoglobin or hematocrit can reflect iron deficiency, B12 or folate issues, inflammation, bleeding, or other causes. High values can appear with dehydration, high altitude, sleep apnea, smoking, or testosterone therapy, and sometimes require a more careful workup.
Helpful references:
Worth following up:
- Low hemoglobin plus symptoms (fatigue, shortness of breath, exercise intolerance)
- High hematocrit that is persistent, especially with headache, flushing, or clot risk factors
MCV and RDW: the “type” of anemia clue
MCV describes average red blood cell size; RDW reflects variation in size. Together, they often point toward nutritional patterns (iron, B12, folate), inflammation, alcohol effects, thyroid patterns, and more.
Worth following up:
- High MCV with low-normal B12 markers, higher alcohol intake, or liver enzyme changes
- High RDW that persists, especially when paired with fatigue or inflammatory markers
Platelets and MPV: clotting and inflammation context
Platelet count and MPV can shift with inflammation, iron deficiency, and other physiologic stressors. Isolated mild abnormalities are often retested, but persistent changes should be interpreted in context.
2) CMP and metabolic markers: kidney, liver, electrolytes
This is where “follow up soon” often matters, because patterns can signal kidney stress, liver workload, or electrolyte imbalance.
Kidney signals: creatinine, eGFR context, urine markers
Creatinine is influenced by hydration and muscle mass, so it is not a perfect standalone “kidney health” number. What you want is context: trend, eGFR, and urine markers when indicated.
Worth following up:
- Rising creatinine compared to your baseline
- Protein or albumin in urine that persists (especially outside of heavy exercise days)
- Abnormal kidney-related markers plus high blood pressure or diabetes risk
Liver enzymes: when to repeat vs investigate
Mild elevations in liver enzymes are common and often reversible (fatty liver risk, alcohol, medications, intense exercise). Follow-up depends on the size of the elevation, persistence, and whether other liver markers move together.
Useful companion context:
Worth following up:
- Enzymes elevated on repeat testing
- A pattern where multiple liver markers trend the wrong direction
- Elevated enzymes with symptoms (abdominal pain, jaundice, dark urine) or high alcohol intake
Electrolytes: sodium and friends
Electrolytes can shift with dehydration, endurance exercise, vomiting or diarrhea, certain medications, and kidney function.
Follow up soon:
- Electrolyte abnormalities that are more than borderline
- Abnormal values with neurologic symptoms (confusion, weakness) or significant GI losses
3) Inflammation markers: “silent” risk vs transient noise
Inflammation markers are easy to overinterpret because they can rise with anything from gum inflammation to a recent cold.
hs-CRP: a cardiovascular and metabolic context marker
High-sensitivity CRP is often used to quantify low-grade inflammation. A single elevated value can be temporary. Persistent elevation is where follow-up becomes valuable, especially alongside lipid risk markers or insulin resistance.
Worth following up:
- hs-CRP elevated on repeat testing when you are well (no infection)
- Elevated hs-CRP plus abnormal ApoB, LDL patterns, or triglycerides
ESR (sed rate): broad, non-specific, still useful
ESR is another inflammation signal. Like hs-CRP, it is not diagnostic alone, but a persistent elevation can justify a deeper look depending on symptoms.
4) Iron and nutrient patterns: common “hidden” drivers of symptoms
If you feel tired, cold, short of breath with exertion, or your training recovery is off, iron and B vitamin patterns are common culprits.
Ferritin and iron saturation: don’t interpret in isolation
Ferritin can be low with iron deficiency, but it can also be high during inflammation. Iron saturation adds clarity, and pairing these with CBC indices can identify patterns earlier.
Worth following up:
- Low ferritin with anemia indices on CBC
- High ferritin plus elevated hs-CRP (consider inflammation as a driver)
- Iron markers that move in opposite directions than expected, which can happen in chronic inflammation
Vitamin B12: normal range vs functional adequacy
B12 status can be tricky because “in-range” does not always align with symptoms, and interpretation often benefits from companion markers (for example, homocysteine).
5) Lipids: “normal” on standard cholesterol, but still worth a deeper look
Standard lipids (total cholesterol, LDL-C, HDL-C, triglycerides) are helpful, but they do not always capture risk, especially if you have a family history of early heart disease.
ApoB and Lp(a): two follow-ups that change the conversation
-
ApoB is a strong indicator of the number of atherogenic particles.
-
Lp(a) is largely genetic and can add risk even when LDL-C looks acceptable.
Worth following up:
- “Normal” LDL-C but strong family history, metabolic risk, or elevated hs-CRP
- Any known elevated Lp(a), because it often shifts prevention intensity
For general cardiovascular risk context and why certain markers matter, the American Heart Association’s overview of cholesterol is a useful starting point.
The 6 questions to ask when something is abnormal
These questions make follow-up faster and more productive:
- Could prep have skewed it? Fasting, hydration, alcohol, intense exercise, illness.
- Is it a one-off or a trend? Compare to prior labs.
- Do related markers agree? Example: AST with GGT, ferritin with hs-CRP, hemoglobin with MCV/RDW.
- Is there a benign explanation worth testing first? Dehydration, recent training block, new medication.
- What is the right retest window? Some issues warrant days to weeks, others months, your clinician can tailor timing.
- What single add-on test would reduce uncertainty most? This is where companion biomarkers are valuable.
A simple follow-up flow you can use every time
How Vitals Vault helps when you want clarity, not guesswork
If your blood work results leave you with more questions than answers, the problem is often not access to testing. It is getting a coherent interpretation, identifying the few numbers that matter most, and tracking whether your changes are working.
Vitals Vault is built for that preventive, longevity-focused workflow: comprehensive panels (100 to 160+ biomarkers), clinician-reviewed insights delivered in days, and daily protocols tailored to your biology. You can test without a referral, upload past reports, and track progress over time. Plans start at $99, are HSA/FSA eligible nationwide, and include a guarantee of at least 3 actionable insights (or your money back).
Learn more at Vitals Vault.
Important safety note
This article is educational and cannot diagnose or treat medical conditions. If your lab report is marked “critical,” or you have concerning symptoms, seek urgent medical care. For non-urgent abnormalities, a clinician can help you choose the right repeat testing and next steps based on your history and medications.
Conclusion
Interpreting blood work requires looking beyond isolated numbers to patterns, trends, and your overall health context. Many flagged results reflect normal biological variability or temporary factors, but persistent or multiple abnormalities merit careful follow-up with your clinician. By understanding what your blood work results indicate and asking the right questions, you can make informed decisions about retesting and care priorities.